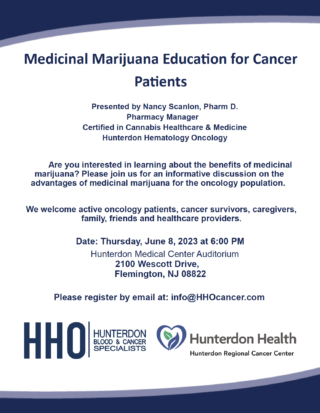
Join Us for an Informative Evening: “Medicinal Marijuana Education for Cancer Patients”
At Hunterdon Hematology Oncology (HHO), we believe in empowering cancer patients with knowledge and providing them with comprehensive care. As part of our commitment to their well-being, we are excited to announce an upcoming community event that aims to shed light on the benefits of medicinal marijuana for the oncology population. We invite you to join us for an informative evening on Thursday, June 8, 2023, at 6:00 PM, in the Hunterdon Medical Center Auditorium at 2100 Wescott Drive, Flemington, NJ 08822.
Cancer patients and their support network face numerous challenges during their treatment journey. At times, traditional treatments may not address all their symptoms or side effects. This is where medicinal marijuana can play a significant role. It has shown promise in alleviating pain, reducing nausea and vomiting, stimulating appetite, and improving sleep quality.
Our “Medicinal Marijuana Education for Cancer Patients” event aims to provide a platform for individuals to learn about the advantages of incorporating medicinal marijuana into their cancer treatment. Whether you are an active oncology patient, a cancer survivor, a caregiver, a family member, a friend, or a healthcare provider, this event is open to all who wish to expand their understanding of this complementary therapy.
We are honored to have Nancy Scanlon, Pharm D., the Pharmacy Manager for Hunterdon Hematology Oncology, as our esteemed presenter. With her expertise and certification in Cannabis Healthcare & Medicine, she will lead an informative discussion on the potential benefits of medicinal marijuana for cancer patients. Nancy’s extensive knowledge and experience make her the ideal resource to address your questions and concerns.
Don’t miss this unique opportunity to engage with experts and learn more about the potential benefits of medicinal marijuana. To ensure your attendance, we encourage you to register in advance by emailing info@hhocancer.com. We look forward to seeing you on June 8th, as we come together to support and empower our community!
To stay updated on our services and future events, visit our homepage at www.hhocancer.com.