Over many decades our understanding of how cancer starts and spreads has steadily improved. However, many myths and misconceptions about cancer remain and can be widespread. Here we try to dispel some of these myths that might cause you undue stress and lead you down the wrong road when learning about cancer.
Does Sugar Make Cancer Grow Faster?
Nope. While we do know that cancer cells “eat” (consume) more sugar than normal cells, there is no scientific evidence that eating more sugar will make your cancer worse, nor that eating less sugar will cause the cancer to grow more slowly. BUT – this is important – excess sugar consumption, which is epidemic in the United States, can increase the level of risk for gaining weight, and we know that obesity is a high risk factor for diabetes and for developing certain kinds of cancer. So, while sugar in itself does not cause cancer, is contributes to the development of conditions that can increase its risk and should be consumed within limits
How About Artificial Sweeteners (Chemicals)?
Nope. Scientists have conducted extensive research into this question and have discovered no evidence that artificial sweeteners cause cancer or cause it to grow faster. Studies have been done on aspartame (Equal®, NutraSweet®); sucralose (Splenda®); saccharin (Sweet ‘N Low®, Sweet Twin®, NectaSweet®); neotame; acesulfame potassium (Sunett®, Sweet One®) and cyclamate and found no evidence of cancer causation. All of these sugar substitutes (except cyclamate) have been approved by the Food and Drug administration.
Does My Attitude Help or Hinder Cancer Growth or Recovery?
A diagnosis of cancer can lead to a wide spectrum of emotions which are all perfectly normal. While your attitude doesn’t directly affect the growth or regression of a tumor, it can be very important in upkeeping physical activity (exercise), nutritional intake, and also maintaining a strong social support network which in turn can make an impact on how treatment is managed. We do know that with a positive attitude the treatment process can be easier to adjust to and can potentially make recovery itself better as well.
Can Biopsy or Surgery of a Cancerous Tumor Cause It to Spread?
Thankfully, the chance of that happening is exceedingly low. Nowadays, surgeons utilize methods and protocols and take many steps to ensure that that does not happen. As an example, if surgeons need to remove tissue from more than one place in the body, they use separate sterilized tools for each location to prevent this very thing from happening.
Is It Possible to “Catch” Cancer?
Not in general. Cancer is not contagious. You can’t “catch” it from another person and it doesn’t spread from person to person like a virus or bacterial illness. Remember, cancer is caused by a genetic mutation. The only exception to this is in the case of an organ transplant where the donor had cancer in that organ. This however doesn’t happen anymore since organ donors are screened for cancer and those organs cannot be donated.
There are certain viruses and bacteria (e.g. human papillomavirus, or HPV, and bacteria such as Helicobacter pylori) that can eventually lead to certain types of cancer. In some cases, like with HPV, there can be person to person transmission of the virus itself but not the cancer that it can lead to
Can My Cell Phone Give Me Cancer?
No, based on the scientific research studies done thus far. Cancer is due to genetic mutation and cell phone’s emission of low-frequency energy does not cause genetic mutations.
Can Power Lines Cause Cancer?
Once again, no, according to all the research done thus far. Just like cell phones, power lines emit low-frequency magnetic energy, and like cell phones, that magnetic energy does not cause genetic mutations. Besides, power lines are well-shielded and weakened by walls in homes or elsewhere.
Do Herbal Remedies Cure Cancer?
Contrary to certain belief systems that are widespread today, there are NO herbal products that cure cancer. There are a few studies that suggest that some herbal remedies may help patients to cope with cancer; however, they do not cure it. Before taking any herbal remedies, discuss it with your oncologist as some herbal products may in fact interfere with the effectiveness of chemotherapy or radiation therapy.
Can I inherit cancer?
90 – 95% of cancers develop because of cellular genetic mutations that take place during the patient’s lifetime – in other words, they are not inherited. They develop from the natural process of aging, or through repeated exposure to a carcinogenic substance in the environment, such as tobacco smoke. However, around 5 – 10% of cancers do result from inheriting a genetic mutation from a parent. In such relatively rare cases, multiple family members may develop the same type of cancer due to the inheritance of the harmful mutated gene from a parent. These are called “inherited” or “familial” cancers. Examples of this can be seen with breast and colon cancers.
Can Deodorants/Antiperspirants Cause Cancer?
In short, no. There is no scientific evidence that links the active ingredients in deodorants and antiperspirants to genetic changes resulting in cancer.
Does Hair Dye Cause Cancer?
To date, there is no scientific evidence that personal use of hair dye increases the risk of cancer. There are studies, however, suggesting that hairdressers/barbers who are more regularly and routinely exposed to hair dye in large quantities may have a greater risk of developing bladder cancer.
If Nobody in My Family Has Cancer, Am I Protected?
No. Remember that cancer develops from spontaneous genetic mutations that occur throughout life due to aging and repeated exposure to certain environmental factors, such as too much sun radiation, smoking tobacco, repeated exposure to dangerous chemicals, how you eat, whether or not you exercise, and simply the process of aging.
Is Cancer Practically a Death Sentence?
Not so fast. That may have been true during decades and centuries gone by. However, starting around the 1990’s, the likelihood of dying from cancer has steadily become less and less. For thyroid, breast and prostate cancers, the survival rate is now 90 percent or better. And the overall survival rate for all cancers combined has increased to around 67 percent.
Of course, this is aggregate data. In any individual case, several factors will alter those statistics, such as the rate of growth of the cancer cells, the degree to which the cancer has spread throughout the body, the availability of certain treatments, and your general health profile.
Sources:
National Cancer Institute: “Common Cancer Myths and Misconceptions”


 At the age of 22, Ashley McRoy was diagnosed with stage 4 colon cancer and given a 20 percent chance of survival. Doctors at Hunterdon Regional Cancer Center made sure she made it to her wedding day — and beyond.
At the age of 22, Ashley McRoy was diagnosed with stage 4 colon cancer and given a 20 percent chance of survival. Doctors at Hunterdon Regional Cancer Center made sure she made it to her wedding day — and beyond.
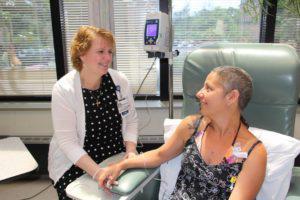 Pictured left to right: Kathy Robbins, RN, MSN, OCN, Clinical Research Nurse at Hunterdon Regional Cancer Center works closely with patients on clinical trials. Kathy talks to Daria Shepherd and provides comfort and education during her treatment at Hunterdon Regional Cancer Center.
Pictured left to right: Kathy Robbins, RN, MSN, OCN, Clinical Research Nurse at Hunterdon Regional Cancer Center works closely with patients on clinical trials. Kathy talks to Daria Shepherd and provides comfort and education during her treatment at Hunterdon Regional Cancer Center.