Exploring the Use of Medicinal Cannabis for Cancer Patients: Pain Relief, Symptom Management, and More
In recent years, medicinal marijuana has gained attention as a complementary therapy for integrated oncology treatment plans, offering potential benefits for symptom management and enhancing the quality of life for cancer patients. Integrating cannabis into modern treatment plans requires a thorough understanding of its applications, administration methods, and the latest findings.
Understanding Medicinal Marijuana in Oncology
Medicinal marijuana, also known as medical cannabis, refers to the use of the Cannabis sativa plant and its cannabinoids—primarily tetrahydrocannabinol (THC) and cannabidiol (CBD)—for therapeutic purposes. In the context of cancer care, cannabis has been explored for its potential to alleviate various cancer-related symptoms and treatment side effects.
Applications of Cannabis in Cancer Care
1. Pain Management
Chronic pain is a common issue among cancer patients. Cannabinoids have shown promise in providing analgesic effects, potentially offering relief when conventional pain medications are insufficient. A study published in the Journal of Clinical Oncology found that cannabis-based medicines may be effective in managing cancer-related pain.
2. Nausea and Vomiting Control
Chemotherapy-induced nausea and vomiting (CINV) significantly impact patients’ quality of life. Cannabis-based medications have been found effective in reducing these symptoms, especially in cases unresponsive to standard antiemetics. The National Cancer Institute (NCI) acknowledges that cannabinoids may help treat nausea and vomiting caused by chemotherapy.
3. Appetite Stimulation
Cancer and its treatments often lead to anorexia and weight loss. Cannabis has been associated with appetite stimulation, which can help counteract weight loss in cancer patients. The American Cancer Society notes that cannabinoids may help improve appetite in patients undergoing cancer treatment.
4. Mood and Sleep Improvement
Anxiety, depression, and sleep disturbances are prevalent among cancer patients. Some studies suggest that cannabinoids may have anxiolytic and sedative properties, potentially improving mood and sleep quality. However, more research is needed to fully understand these effects.
Administration Methods
Medicinal cannabis can be administered through various methods, each with its own onset time and duration of effects:
- Oral Ingestion: Cannabis-infused edibles, capsules, or oils are ingested orally, leading to slower onset but longer-lasting effects. However, dosing can be challenging due to variability in absorption and metabolism.
- Inhalation: Vaporizing cannabis allows for rapid onset of effects. However, smoking is generally not recommended due to potential respiratory risks.
- Sublingual Administration: Tinctures or sprays applied under the tongue offer relatively quick absorption and onset of effects, providing an alternative to inhalation.
- Topical Application: Cannabis-infused creams or balms can be applied directly to the skin to target localized pain or inflammation, though systemic effects are minimal.
Considerations and Precautions
While medicinal marijuana presents potential benefits, it is essential to consider possible side effects and interactions:
- Psychoactive Effects: THC, the primary psychoactive component, can cause euphoria, dizziness, or anxiety in some individuals. Starting with low doses and titrating slowly can help mitigate these effects.
- Cognitive Impairment: Long-term use of cannabis has been associated with cognitive impairments, including memory and attention deficits. Patients should be monitored regularly to assess cognitive function.
- Drug Interactions: Cannabinoids may interact with other medications metabolized by the liver. It is crucial to consult with healthcare providers to evaluate potential interactions.
- Legal and Regulatory Considerations: The legal status of medicinal marijuana varies by region. Patients and providers must be aware of local regulations to ensure compliance.
Integrating medicinal marijuana into oncology treatment plans offers a promising avenue for enhancing patient care. However, it requires careful consideration of individual patient needs, potential benefits, and risks. Collaboration between patients and healthcare providers is essential to develop personalized, safe, and effective treatment strategies.
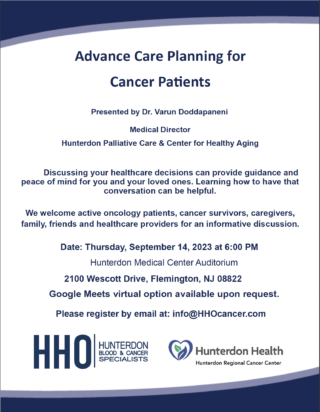
Hunterdon Hematology Oncology remains committed to providing our patients and community with the latest information on innovative cancer care options. Working closely with Hunterdon Regional Cancer Center, we offer educational support events to empower patients, caregivers, and healthcare professionals with valuable knowledge. A recent example is our Medicinal Cannabis session, led by Nancy Scanlon, Pharm D., our Pharmacy Manager and a certified expert in Cannabis Healthcare & Medicine (view the recording here). Events like these ensure that our community has access to evidence-based discussions on emerging therapies, helping patients make informed decisions about their care. Stay connected with us for future events and resources designed to support you and your loved ones on your journey.