Power in Meditation: A Path to Healing for Patients and Their Loved Ones
Why Mindfulness Matters in the Cancer Journey
A cancer diagnosis can be an overwhelming experience—not just for the patient but also for caregivers, family members, and loved ones who provide unwavering support. While medical treatments focus on targeting the disease, emotional and mental well-being play a critical role in the overall healing process.
One effective, science-backed approach to managing the emotional and physical challenges of cancer is meditation for cancer patients and their support networks. Mindfulness and meditation techniques have been shown to reduce stress, improve sleep, alleviate anxiety, and enhance overall quality of life during cancer treatment and survivorship.
How Meditation Supports Patients
Meditation, particularly mindfulness-based stress reduction (MBSR), guided imagery, and breathwork, has been studied extensively for its positive effects on cancer patients. Many top cancer centers in the U.S., including Memorial Sloan Kettering Cancer Center and MD Anderson Cancer Center, offer mindfulness and meditation programs as part of integrative cancer care.
Here’s how a regular meditation practice can benefit patients:
1. Reduces Stress and Anxiety
Cancer treatments such as chemotherapy, radiation, and immunotherapy can cause physical and emotional stress. Meditation helps lower cortisol levels, the hormone responsible for stress, leading to a greater sense of calm. According to a study published in the Journal of Clinical Oncology, mindfulness meditation has been associated with significant reductions in anxiety and depression in cancer patients.
2. Improves Sleep Quality
Cancer-related fatigue and insomnia are common struggles during treatment. Research from the National Cancer Institute (NCI) suggests that mindfulness meditation can help regulate sleep patterns, allowing patients to rest more effectively, which is essential for recovery.
3. Helps with Pain Management
Pain from cancer treatments can be debilitating, but meditation activates regions in the brain associated with pain control. A study from Harvard Medical School found that meditation can help patients develop a greater tolerance for discomfort by shifting their focus away from pain.
4. Strengthens Emotional Resilience
Mindfulness practices help patients cultivate emotional resilience by encouraging acceptance and self-compassion. This can be especially beneficial for individuals undergoing long-term treatment, as it provides them with coping mechanisms to navigate uncertainty and fear.
Meditation for Caregivers and Family Members
Cancer doesn’t only impact the patient; it also affects those providing care and support. Caregivers, family members, and friends often experience emotional exhaustion, stress, and even burnout. Practicing meditation can help them find balance while ensuring they are mentally and emotionally available for their loved one.
1. Prevents Caregiver Burnout
According to the American Cancer Society, caregivers often experience high levels of emotional and physical fatigue. Engaging in short meditation sessions—such as mindful breathing or guided relaxation—can help reduce chronic stress and overwhelm, improving the caregiver’s ability to provide support.
2. Enhances Emotional Connection
When loved ones practice mindfulness, they become more present and engaged in the patient’s journey. This fosters deeper connections, better communication, and a greater sense of understanding between patients and caregivers.
3. Encourages Self-Care and Inner Peace
Caregivers frequently put their own needs last. However, prioritizing self-care through meditation allows them to recharge and regain clarity, ensuring they are in the best possible state to help their loved one.
Simple Meditation Techniques for Patients and Caregivers
Starting a meditation practice doesn’t require hours of dedication. Here are a few easy mindfulness techniques that patients and caregivers can incorporate into their daily routine:
1. Guided Meditation
Listening to a meditation app like Calm, Headspace, or Insight Timer can provide structured guidance for relaxation and stress relief. Many cancer centers also offer recorded meditations tailored for oncology patients or referrals to local organizations that hold sessions.
2. Deep Breathing Exercises
Practicing diaphragmatic breathing (deep belly breathing) for just 5-10 minutes a day can help regulate the nervous system and lower stress. Try the 4-7-8 breathing technique (inhale for 4 seconds, hold for 7, exhale for 8) to promote relaxation.
3. Body Scan Meditation
This technique involves focusing on different areas of the body, releasing tension, and noticing physical sensations. Studies from Johns Hopkins Medicine suggest that body scan meditation can help with pain perception and relaxation in cancer patients.
4. Jin Shin Jyutsu Energy Healing
Jin Shin Jyutsu, a simple yet powerful energy healing technique, involves placing the hands on specific points of the body to restore balance. It can be used alongside meditation to help relieve stress and promote well-being.
Incorporating Meditation into Care
Many hospitals and cancer treatment centers now recognize mindfulness-based interventions as valuable complementary therapies. Patients and caregivers interested in incorporating meditation into their cancer care plan should speak with their oncology team, social workers, or integrative medicine specialists to explore available programs and resources.
Organizations such as The Elixir Fund offer meditation workshops designed specifically for cancer patients and caregivers.
Join HHO for a Guided Meditation
At Hunterdon Hematology Oncology, we believe in providing holistic support for our patients and their families. If you’d like to experience the benefits of meditation firsthand, we invite you to join us on Tuesday, April 22, 2025, at 5:00 PM at the Hunterdon Medical Center Auditorium (2100 Wescott Drive, Flemington, NJ 08822) for a special guided meditation session led by Meg McQuarrie, Executive Director of The Elixir Fund.
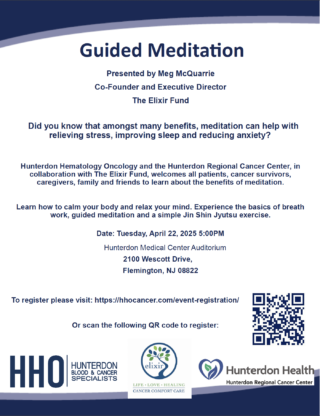
This in-person event will introduce attendees to breath work, guided meditation, and a simple Jin Shin Jyutsu exercise to help relieve stress and promote healing.
Reserve your spot today at: www.hhocancer.com/event-registration/
Final Thoughts
A daily meditation practice can be a powerful tool for emotional healing and stress reduction during cancer treatment. Whether you are a patient, a survivor, or a caregiver, taking time for mindfulness can significantly improve your overall well-being. By incorporating meditation into your routine, you can foster resilience, inner peace, and a sense of control throughout your journey.
Would you like to learn more about meditation and other wellness resources for cancer patients? Visit our blog regularly or follow us on social media for more upcoming events and support programs!