You may have heard of immunotherapy, and at least understand that it represents a huge advancement in the treatment of cancer. You may also know that, in broad terms, immunotherapy works by helping the patient’s own immune system work more effectively in finding, attacking, and killing cancer cells. To learn more about what immunotherapy is, and how it works, click here.
Because immunotherapy simply trains the patient’s immune system to work more effectively, you might also think that immunotherapy has no side effects. What we are finding, however, is that that belief is incorrect. Immunotherapy does have a spectrum of side effects. Immunotherapy patients experience side effects approximately 5-10% of the time, and these cases of side effects are life-threatening around 1-2% of the time. Being forewarned is forearmed, so let’s explore the types of immunotherapy side effects that can occur.
Most common side effects: Fatigue & Inflammation
Just like other kinds of cancer treatment, fatigue is one of the most common side effects. Feelings of overall low energy, and/or becoming exhausted quickly and easily when exertion is required, are very common side effects. This kind of physical debilitation can occur within just a few weeks of commencement of treatment but can sometimes not happen until several months – or even years – have passed. Generally, this side effect tends to get better with enough passage of time. However, while this side effect does generally improve with the passage of time, you may not return 100% to your former levels of overall energy or stamina levels. There may be some lingering, low-level fatigue that remains.
Immunotherapy medications can also cause a variety of inflammations throughout the body. Skin inflammation can manifest as a rash, feeling itchy, or as pigment changes, sometimes without a rash. Inflammation of the colon may occur, causing diarrhea and/or abdominal pain. Inflammation of the lungs can occur, causing chest pain and a cough.
Rarer side effects: Diabetes, Endocrine system problems, and Hypophysitis
Side-effects that more rarely occur include development of diabetes (a chronic condition that negatively impacts how the body processes glucose, or in more severe cases, progresses to the point that the pancreas produces little-to-no insulin, the critically important hormone which regulates the amount of glucose in the blood).
Another rarely occurring side effect is damage to the body’s endocrine system, responsible for how the body produces and regulates hormones – all hormones, not just insulin. Another rare, but more concerning side effect is the inflammation of the pituitary gland, known as hypophysitis. Hypophysitis manifests in many different ways, so a definitive diagnosis requires blood work. Symptoms include headache, fever, or fatigue.
Side effects do not depend on cancer type
The side effects described above do not generally depend on the patient’s type of cancer. Rather, they depend more on the type of immunotherapy medication prescribed for cancer treatment.
Management of side effects
Research has found that the most appropriate treatment for the various side effects that occur depends on the severity of the effect. Many patients receiving immunotherapy have already received chemotherapy, so they have most likely already experienced the milder side effects like fatigue, rash, and/or cough. As a result, they have already developed the necessary coping skills and/or method of treatment for them.
When it comes to diarrhea, however, treatment approach is critical. The most highly preferred treatment approach is modification of diet. Limiting dairy products can be very important in this case. The reason that dietary changes are preferred is that anti-diarrheal medications can cause severe, even life-threatening, complications. If the diarrhea problem is severe, your doctor may recommend a temporary cessation of immunotherapy, and replacement with an immunosuppressant. This can help to reduce the inflammation behind the diarrhea to a safer level, yielding improvement in diarrheal symptoms.
Patients who develop diabetes may also require a temporary pause on the immunotherapy drugs, combined with insulin medication treatment. In any case, the temporary pause can help the body to recover, heal, and reduce the severity and/or existence of unwanted side effects. The ultimate goal, however, is to resume immunotherapy treatment; to attack and kill the tumor’s cancer cells.
Side effects have nothing to do with immunotherapy effectiveness
Patients often believe that the presence and severity of side effects is also a measure of the effectiveness of the immunotherapy treatment. This is not true. Patients whose immunotherapy treatment is highly effective often experience no side effects. This can lead them to suspect that they are only receiving a placebo medication in a secret clinical trial, or that the immunotherapy medication isn’t working at all. This is simply not true. Remember: only 5-10% of immunotherapy patients experience any side effects. So, 90-95% of immunotherapy patients have no side effects whatsoever!
Self-awareness is critical
So, the most important advice you can receive relative to the presence or absence of side effects is heightened self (and body) awareness. Pay attention to what your body is trying to tell you, right from the get-go! Make sure that your doctor, as well as your pharmacist, spend lots (and lots) of time with you, going over all the possible side-effects associated with your immunotherapy medication, and make sure you fully understand everything they are saying to you. Ask as many questions as you feel you need to and do not assume that you are a “burden” to them. After all, this is your treatment, and this is your life! You are the one whose life and well-being are being affected. It is your responsibility to ensure that you are completely comfortable with every aspect of your treatment. It is your doctor’s responsibility to ensure that you are, indeed, fully comfortable with all aspects of your treatment.



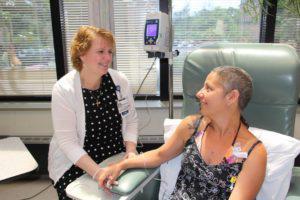 Pictured left to right: Kathy Robbins, RN, MSN, OCN, Clinical Research Nurse at Hunterdon Regional Cancer Center works closely with patients on clinical trials. Kathy talks to Daria Shepherd and provides comfort and education during her treatment at Hunterdon Regional Cancer Center.
Pictured left to right: Kathy Robbins, RN, MSN, OCN, Clinical Research Nurse at Hunterdon Regional Cancer Center works closely with patients on clinical trials. Kathy talks to Daria Shepherd and provides comfort and education during her treatment at Hunterdon Regional Cancer Center.